Picture this: Your hospital just invested millions in state-of-the-art AI systems. You have diagnostic imaging that spots pneumonia faster than ever, clinical alerts that flag potential sepsis cases, and automated systems handling basic administrative tasks. The technology works brilliantly—yet your physicians are still drowning in paperwork, care coordination remains a nightmare, and patient satisfaction scores haven’t budged.
Sound familiar? You’re not alone. This scenario plays out daily across healthcare organizations worldwide, highlighting a fundamental disconnect between AI’s promise and its real-world impact. The problem isn’t that healthcare AI doesn’t work—it’s that most healthcare organizations are still using traditional AI approaches designed for simpler, more predictable industries.
Healthcare needs something different. Something that can think, plan, and coordinate across the messy complexity of patient care. That’s where agentic AI comes in.
What makes healthcare AI so complicated?
Before diving into solutions, let’s acknowledge why healthcare AI is uniquely challenging. Unlike e-commerce recommendations or financial fraud detection, healthcare involves life-and-death decisions where context matters enormously.
Consider a seemingly simple scenario: An elderly patient with diabetes visits the emergency department with chest pain. Traditional AI systems might excel at individual tasks—the ECG AI flags potential cardiac issues, the lab AI notes elevated troponin levels, and the imaging AI identifies subtle changes. But who coordinates these findings with the patient’s medication history, recent hospital visits, family preferences, and insurance coverage? Currently, that burden falls on already overwhelmed clinical staff.
Healthcare data creates another layer of complexity. A single patient generates information across multiple formats: medical images, lab results, clinical notes, sensor data from wearables, social determinants of health, and family history. According to research published in the Journal of the American Medical Informatics Association, healthcare organizations struggle to integrate these diverse data streams effectively, creating information silos that limit AI’s potential impact.
The regulatory environment adds yet another dimension. HIPAA compliance requirements extend beyond basic data protection to encompass audit trails, patient consent management, and explainable decision-making. When the FDA evaluates AI-enabled medical devices , they assess not just accuracy but safety across diverse patient populations and long-term performance reliability.
Traditional AI: powerful but isolated
Most healthcare AI implementations today follow the traditional approach – highly specialized systems that excel at specific tasks but operate in isolation. Think of them as brilliant specialists who don’t communicate with each other.
These systems have achieved impressive results in their narrow domains. Medical imaging AI can achieve accuracy rates exceeding 90% for specific conditions like diabetic retinopathy or lung nodule detection. Clinical decision support systems successfully flag potential drug interactions and alert clinicians to critical lab values.
But here’s the challenge; healthcare isn’t a series of isolated tasks—it’s an interconnected system where every decision ripples across multiple departments, providers, and care episodes. Traditional AI requires human interpreters to connect the dots, coordinate responses, and manage the handoffs between different systems.
A real-world example illustrates this limitation. A patient arrives at the emergency department with multiple chronic conditions. The triage AI assesses urgency, the lab AI analyzes blood work, the pharmacy AI checks for drug interactions, and the imaging AI reviews X-rays. Each system generates valuable insights, but coordinating these findings into a comprehensive care plan requires significant human effort. The result? Clinicians spend valuable time interpreting and integrating AI outputs rather than focusing on patient care.
Healthcare organizations report mixed results with traditional AI ROI, not because individual tools lack value, but because the effort required to coordinate multiple point solutions often outweighs their benefits.
Enter agentic AI: coordination at scale
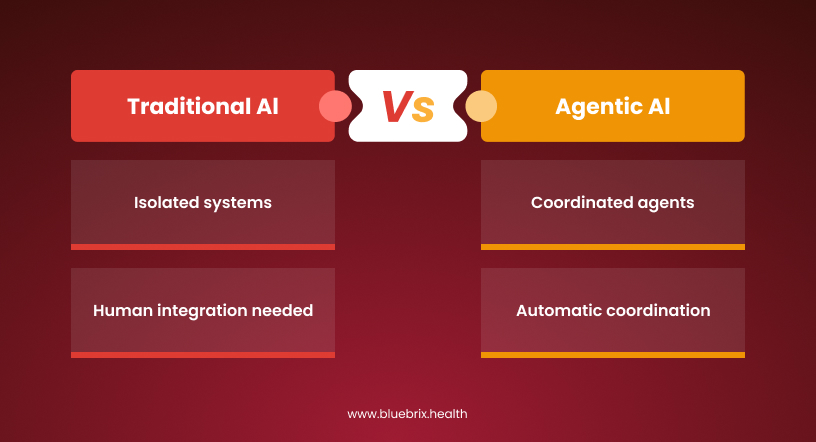
Agentic AI represents a fundamentally different approach. Instead of waiting for human coordination, these systems can reason across multiple healthcare domains, plan multi-step interventions, and execute coordinated responses autonomously.
Think of agentic AI as having a digital care coordinator that never sleeps, never forgets, and can simultaneously manage hundreds of complex cases. Unlike traditional AI that analyzes and reports, agentic AI analyzes, plans, acts, and learns—all while maintaining appropriate human oversight and regulatory compliance.
The architecture differs significantly from traditional approaches. Rather than isolated systems requiring human integration, agentic AI employs multiple specialized agents that communicate and coordinate automatically. A patient with complex needs might have dedicated agents for medication management, appointment coordination, care team communication, and symptom monitoring—all working together under an overarching coordination framework.
Early implementations are showing remarkable results. Academic research demonstrates AI agents achieving over 93% accuracy in complex medical scenarios while coordinating care across multiple specialties. More importantly, these systems can process thousands of cases simultaneously while maintaining detailed audit trails and explainable decision-making.
Real-world results: what’s actually working
The difference between traditional and agentic AI becomes clear when examining real-world implementations and their measurable impacts.
Traditional AI success stories focus on specific workflow improvements. Medical imaging AI reduces radiologist reading time, clinical decision support flags critical conditions, and basic automation handles routine administrative tasks. These improvements are valuable but incremental.
Agentic AI implementations show comprehensive transformation. Recent studies in healthcare AI demonstrate systems that go beyond simple transcription to actively manage entire documentation workflows, update relevant systems, and trigger appropriate follow-up actions. Independent evaluations show that healthcare organizations report significant time savings when implementing comprehensive AI documentation systems.
Revenue cycle management provides another compelling example. Research indicates that advanced autonomous systems can achieve high automation rates in complex billing processes. Unlike traditional AI that might automate individual coding tasks, these agentic systems manage entire claims lifecycles, prevent denials before submission, and adapt strategies based on payer-specific patterns.
Population health management showcases agentic AI’s coordination capabilities. Healthcare organizations implementing autonomous patient monitoring and intervention systems report significant improvements in care coordination and patient outcomes. These systems don’t just identify at-risk patients—they autonomously coordinate outreach, schedule appropriate interventions, and monitor outcomes across entire populations.
Navigating the regulatory landscape
Healthcare leaders often express concern about deploying more autonomous AI systems given the complex regulatory environment. However, regulatory frameworks are evolving to accommodate these new capabilities while maintaining appropriate oversight.
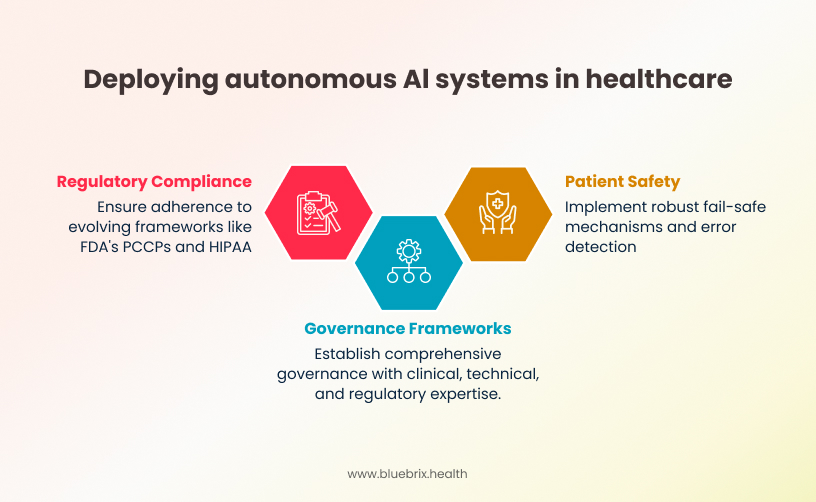
The FDA’s January 2025 guidance on AI-enabled medical devices introduces predetermined change control plans (PCCPs) that allow pre-approved modifications to AI systems. This framework better accommodates agentic AI’s adaptive capabilities while maintaining safety oversight.
HIPAA compliance for agentic AI requires careful consideration but is entirely achievable. The key lies in designing systems with privacy-by-design principles, maintaining comprehensive audit trails across multi-agent interactions, and ensuring appropriate access controls for autonomous decision-making processes.
Patient safety considerations actually favor well-designed agentic AI systems. Unlike traditional AI where errors might go unnoticed until human review, agentic systems can implement robust fail-safe mechanisms, automated error detection, and the ability to roll back autonomous actions when problems are identified.
Forward-thinking healthcare organizations address regulatory challenges through comprehensive governance frameworks that include clinical, technical, and regulatory expertise while implementing continuous monitoring systems that track both individual agent performance and multi-agent coordination effectiveness.
Making the strategic choice: traditional vs agentic AI
Healthcare leaders evaluating AI investments need a clear framework for choosing between traditional and agentic approaches based on their organization’s specific needs and readiness level.
Start with organizational readiness: Traditional AI implementations require basic data infrastructure and change management capabilities. Agentic AI demands more sophisticated preparation; robust data governance frameworks, API-ready system architecture, and staff comfortable with AI-human collaboration models.
Consider your most pressing challenges: Traditional AI excels in well-defined, high-impact applications; medical imaging analysis, clinical decision support for specific conditions, and basic administrative automation. These implementations can show results within 6-12 months and build organizational AI literacy.
Agentic AI shows strongest potential for complex coordination challenges: revenue cycle management, care pathway optimization, population health management, and multi-specialty care coordination. These implementations require 12-24 months but deliver more comprehensive transformation.
Evaluate implementation partnerships: Healthcare industry analysis shows that successful AI implementations often use vendor partnerships rather than building in-house solutions. This hybrid approach provides access to specialized expertise while maintaining organizational control—particularly important for agentic AI systems that require deep healthcare domain knowledge combined with cutting-edge technical capabilities.
The most successful healthcare organizations adopt a hybrid strategy – implementing traditional AI for immediate, well-defined needs while building capabilities for agentic AI deployment in complex 66coordination scenarios.
Building your agentic AI roadmap
The transition to agentic AI capabilities requires strategic planning and phased implementation. Organizations that treat this as simply deploying more sophisticated AI tools often struggle, while those that recognize it as a fundamental operating model shift achieve significantly better outcomes.
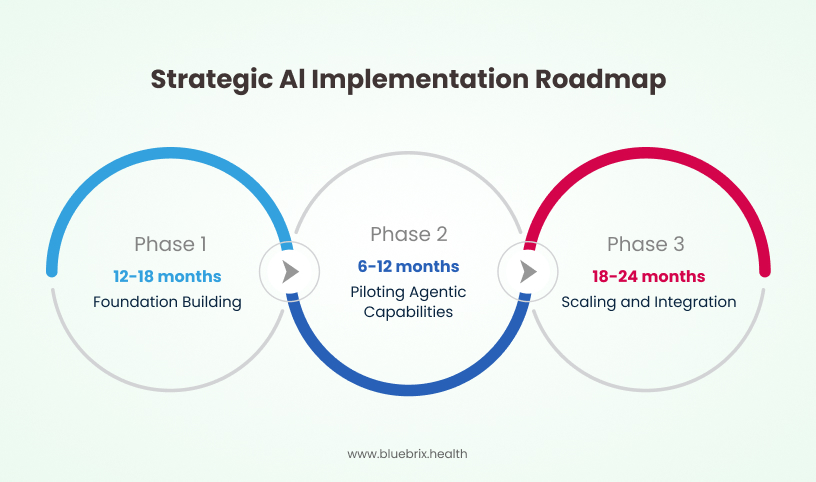
Phase 1: Foundation Building (12-18 months)
Focus on data infrastructure, governance frameworks, and staff AI literacy. Implement proven traditional AI applications—ambient documentation, clinical decision support, basic administrative automation—while establishing the data integration and governance capabilities that agentic AI requires.
Phase 2: Piloting Agentic Capabilities (6-12 months)
Introduce autonomous coordination in controlled environments. Revenue cycle management, care pathway optimization, and population health management represent ideal starting points because they involve complex workflows but lower direct patient safety risks.
Phase 3: Scaling and Integration (18-24 months)
Deploy agentic AI across core clinical and operational functions. By this point, organizations have developed internal expertise, established governance frameworks, and proven ROI from earlier implementations.
The key insight from successful implementations is that agentic AI requires significant change management investment. Staff need time to develop trust in autonomous systems, processes need redesign to accommodate AI coordination, and governance frameworks need updating to address autonomous decision-making scenarios.

