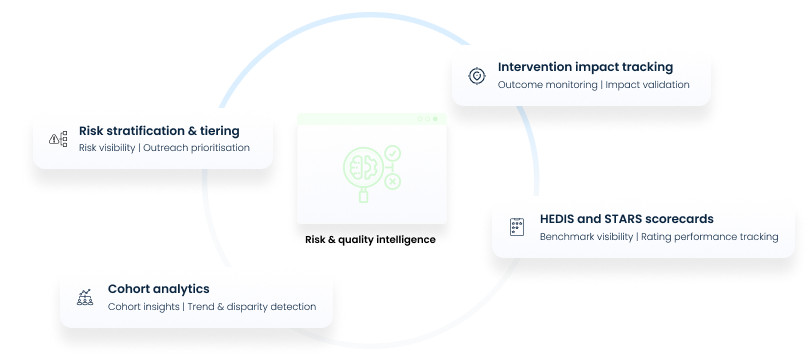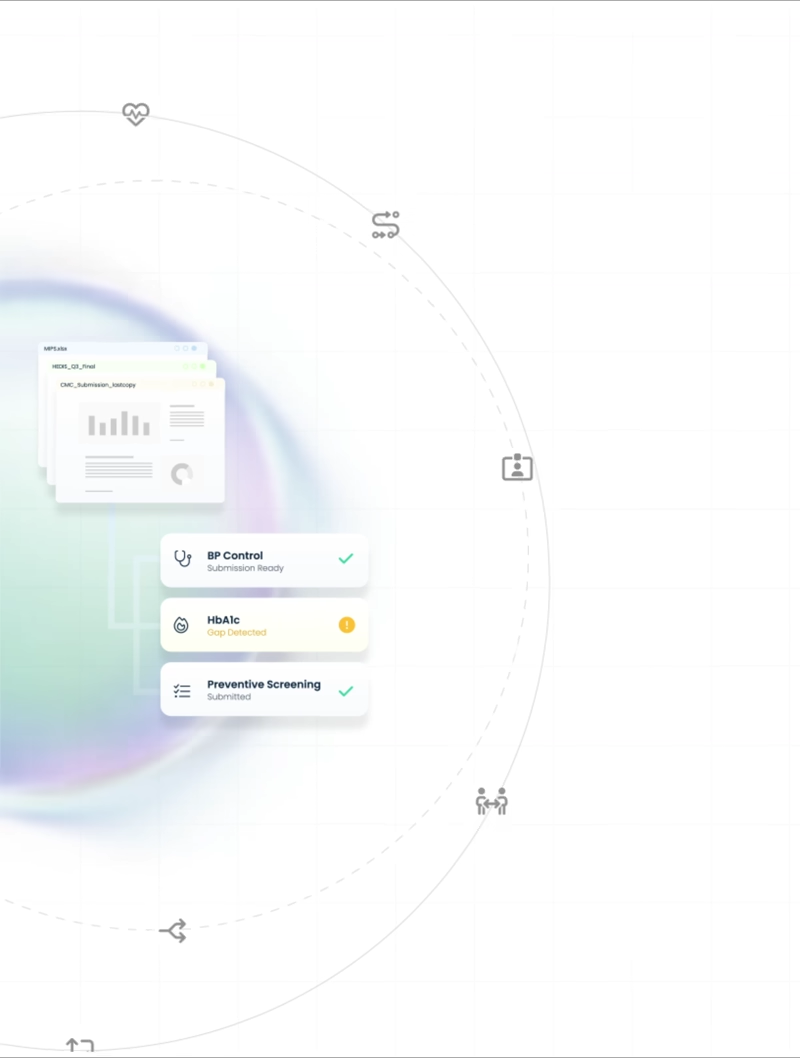
Measure-ready reporting, built into care workflows
Operational, quality, and value-based measures are captured as care is delivered—so CMS, Medicare, and payer reporting is always complete, traceable, and submission-ready.
Cut reporting effort by up to 70% and save 8–12 hours weekly per compliance lead
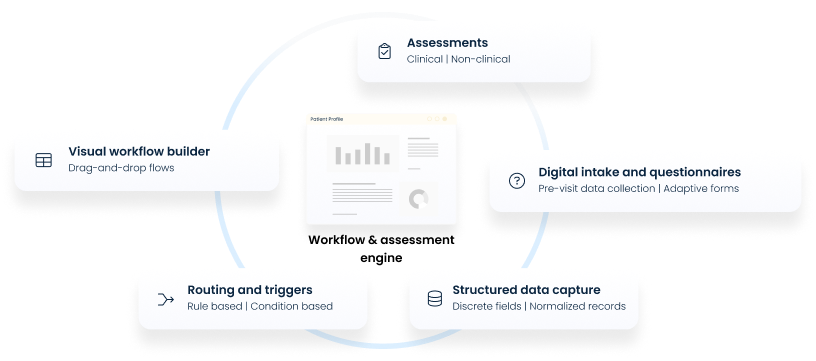
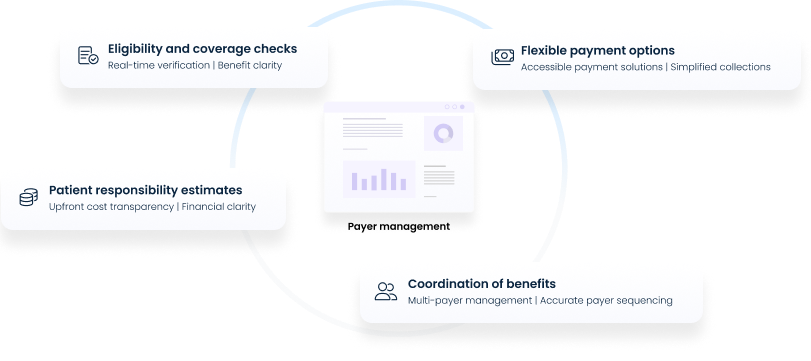
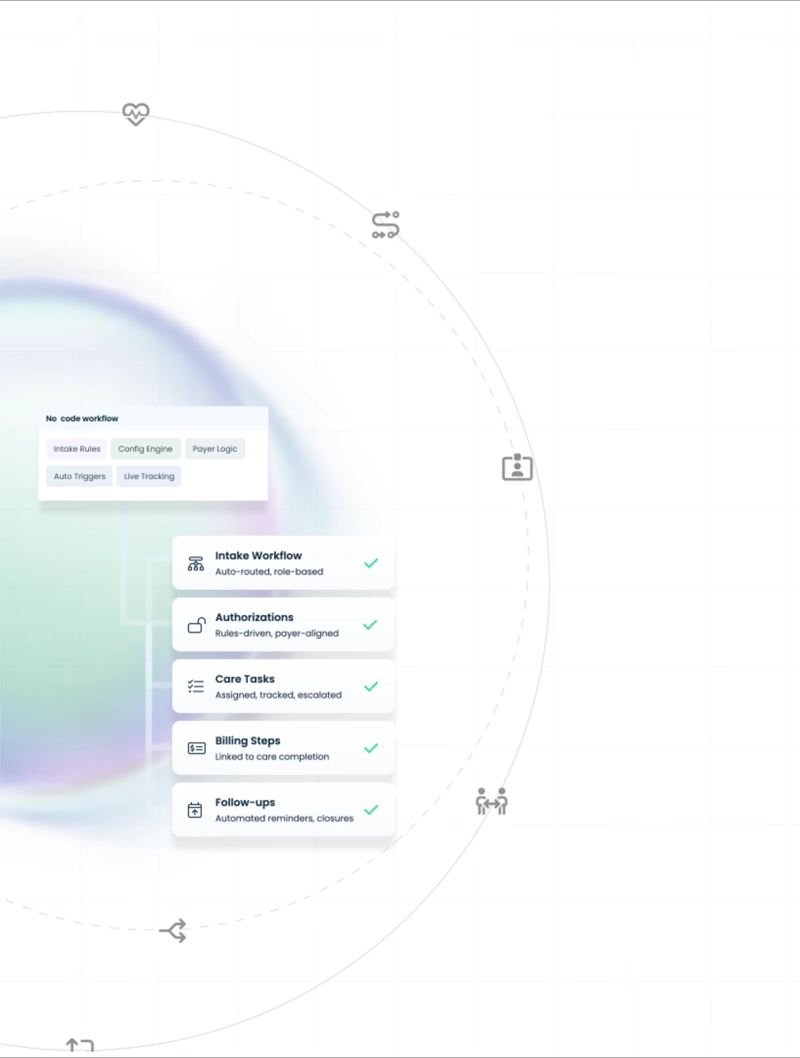
Flexible workflows that align care, operations, and compliance
Get workflows configured aligned to how your teams actually work across intake, care planning, delivery, and billing without rigid processes.
Lower administrative effort by 30–45% while reducing handoffs and rework
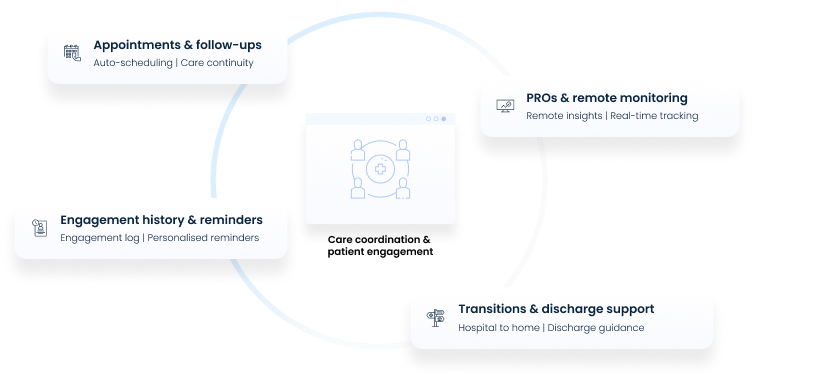
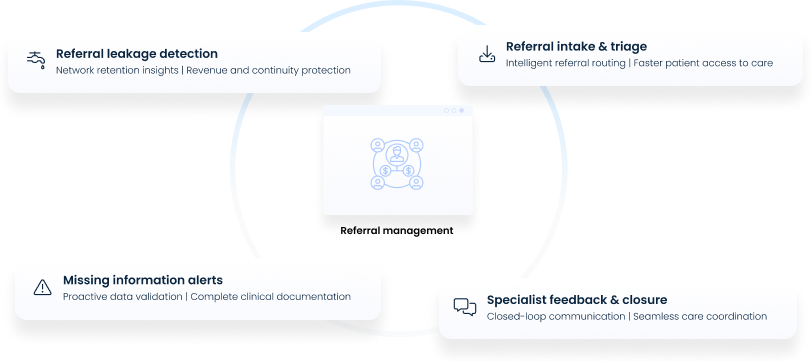
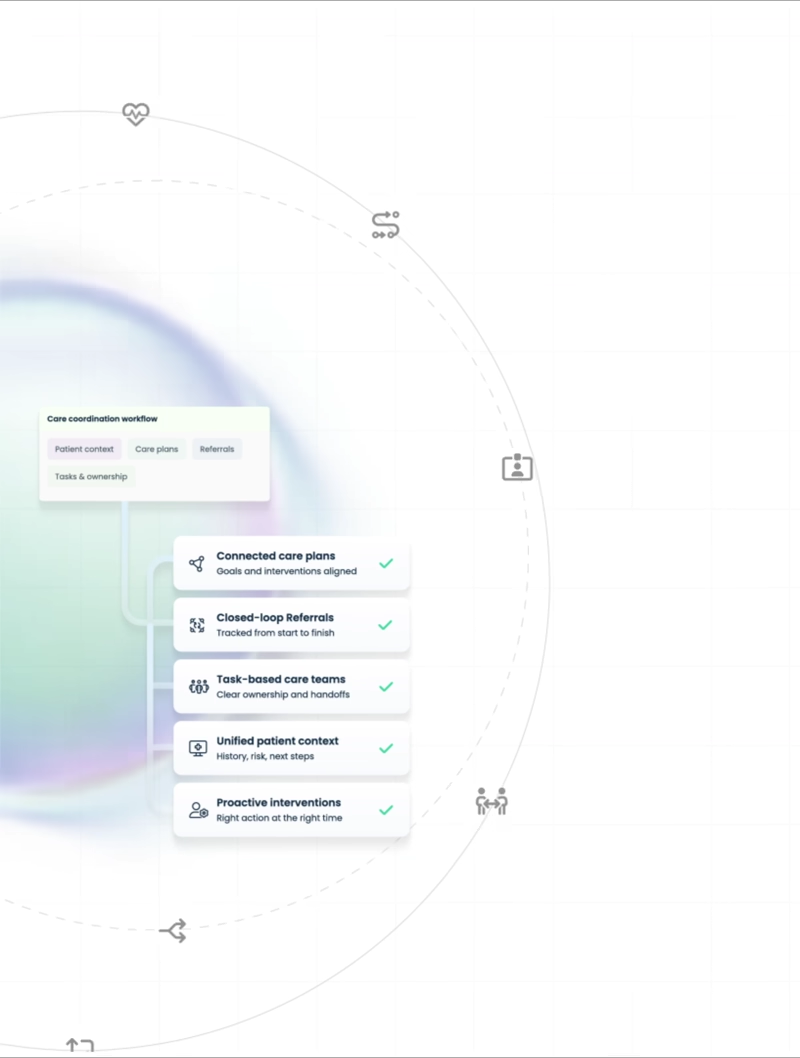
Keeping care teams and patients aligned throughout care delivery
Coordinate care plans, referrals, follow-ups, and patient touchpoints across teams and settings ensuring continuity beyond individual encounters.
Enable coordinators to manage 30–40% more patients without increasing burnout
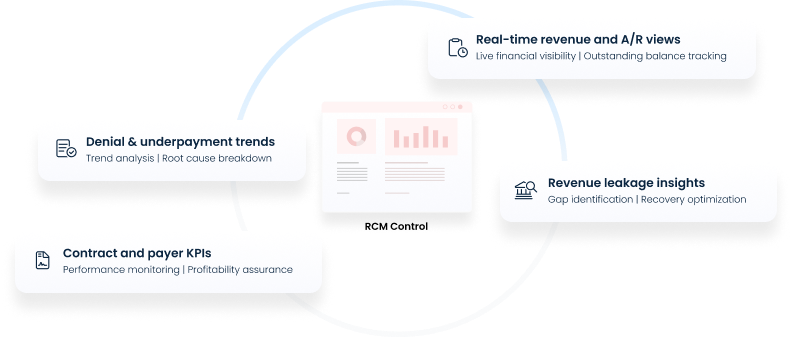
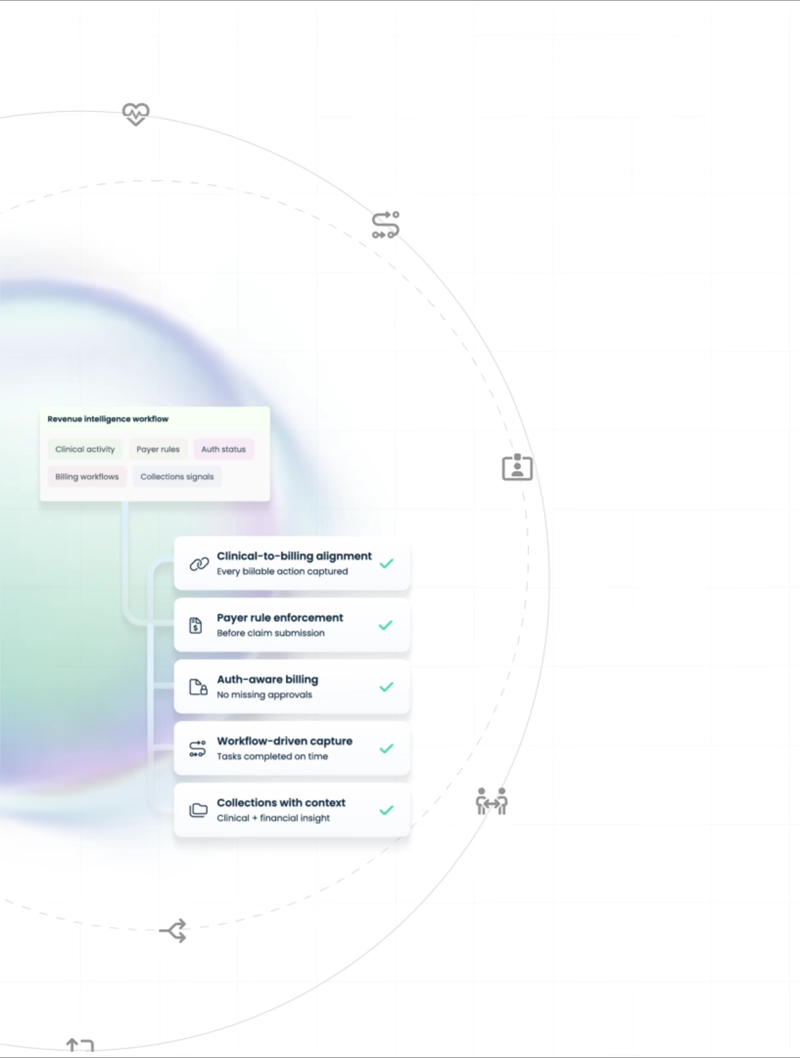
Revenue visibility that starts with care delivery
Connect clinical activity, payer rules, billing, and collections to see where revenue is earned, delayed, or at risk.
Reduce claim denials by 15–25% and accelerate cash flow
Four operational pillars. One care management system
Measure-ready reporting, built into care workflows
Operational, quality, and value-based measures are captured as care is delivered—so CMS, Medicare, and payer reporting is always complete, traceable, and submission-ready.
Cut reporting effort by up to 70% and save 8–12 hours weekly per compliance lead
Flexible workflows that align care, operations, and compliance
Get workflows configured aligned to how your teams actually work across intake, care planning, delivery, and billing without rigid processes.
Lower administrative effort by 30–45% while reducing handoffs and rework
Keeping care teams and patients aligned throughout care delivery
Coordinate care plans, referrals, follow-ups, and patient touchpoints across teams and settings ensuring continuity beyond individual encounters.
Enable coordinators to manage 30–40% more patients without increasing burnout
Revenue visibility that starts with care delivery
Connect clinical activity, payer rules, billing, and collections to see where revenue is earned, delayed, or at risk.
Reduce claim denials by 15–25% and accelerate cash flow